Oxygen. We love it, and it keeps us alive. The atmosphere contains 21 percent oxygen, and we exhale, on average, 16 percent. Thus, with the billions and billions of cells within our body, they operate using only 5 percent of the oxygen we intake. Simply amazing! As efficient as the body is, unfortunately, it is not immune to disease – some of which cause hypoxemia and/or hypoxia. The remedy? Administration of supplemental medical oxygen! Easy, right?
This concept has been taught in initial and continuing education classes for years and written into protocol after protocol with the mindset “more oxygen is better”. A pulse oximetry reading as close to 100% as possible is the gold standard, and achieving anything less than that is considered inadequate patient care. So, how can oxygen, something we all need to survive, be such a bad thing?
For example, if a patient suffers from respiratory distress or hypoxia, why not give as much as possible? The answer is: respiratory distress/hypoxic patients SHOULD always receive supplemental oxygen, but only to the point of re-establishing normal saturations. Currently, the AHA recommends maintaining SpO2 saturation readings between 94 to 99 percent.5 Continuing oxygen delivery outside this parameter is not helpful, and likely, very harmful.
Research shows that time and time again, that routine and unchecked high-flow oxygen administration reaches toxic internal levels within minutes. To this extent, the current European Society of Cardiology guidelines recommends giving oxygen only when oxygen saturation levels are below 90 percent, but not above.1However, despite updated education standards, many EMS providers are still resistant to change their tried and true method of excessive oxygen delivery to ALL patients, especially those experiencing chest pain.
Here are essential points to remember about hyperoxia:
- One, there are three significant consequences of routine, excessive oxygen administration: nitrogen washout, oxygen toxicity, and oxidative stress.
- Two, the atmosphere contains roughly 78 percent nitrogen, thus making up the majority of the volume within the lower airways and alveoli.
- Three, understand that chemically, oxygen is unstable. Within its atomic structure, two pairs of electrons are continually searching for a partner, doing anything to get one – even if it requires stealing from the tissue.
Nitrogen Washout
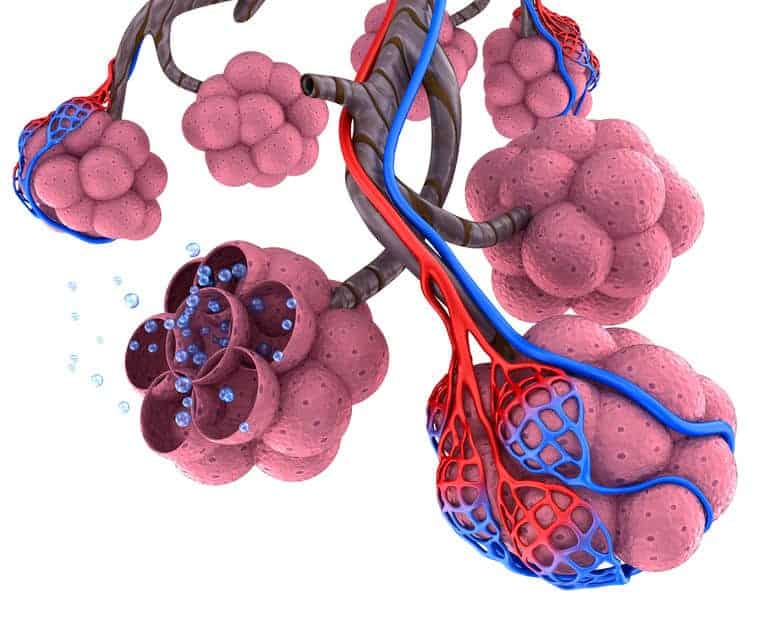
When a patient inhales atmospheric air, oxygen diffuses from the alveoli into the blood, but nitrogen remains within the alveoli. As a result, the residual nitrogen creates enough pressure to keep the alveoli inflated. Therefore, even though oxygen transfers into the blood from the alveoli, the alveoli don’t collapse.
When providing oxygen at concentrations higher than 50 percent, it replaces nitrogen as the primary gas in the lower airways and alveoli.3 As oxygen administration continues, the volume of inspired nitrogen (and its level within distal alveoli) diminishes significantly. With the nitrogen washed out, the gas that helps to keep alveoli inflated is eliminated, and alveoli begin to collapse. Thus, at higher oxygen levels, fewer alveoli are available to participate in gas exchange. As more and more alveoli collapse, atelectasis sets in. This situation rapidly results in ineffective external respiration and the development of hypoxemia.
Oxygen Toxicity
Clinically, the EMS professional observes this and increases the oxygen flow, hoping to relieve the resultant anxiety and developing dyspnea. What begins is a vicious cycle that leads to pulmonary dysfunction and anatomical damage: The patient progressively inhales higher oxygen concentrations as the flow is increased, causing more and more previously functional and intact alveoli to collapse. This increasing atelectasis further decreases lung surface area for the transfer of oxygen into the blood. The hypoxemia worsens, and oxygen flow is increased, and so on.
Here is another complication that develops from excessive oxygen levels within the alveoli: There are alveolar cells called Type 1 and Type 2 (easy enough, right?) Type 1 cells make up the alveolar epithelium (alveolar wall). Type 2 cells make and secrete surfactant and function as stem cells for maintaining the alveolar epithelium (i.e., Type 2 cells make Type 1 cells). As the alveoli collapse from the nitrogen depletion and oxygen exodus, the epithelium (Type 1 cell) is damaged. This damage stimulates Type 2 cells to proliferate and subsequently differentiate, to try and replace the injured Type I cells. Additionally, a portion of the Type 2 cell population becomes abnormally enlarged.4 The side effects of this are a thickening of the alveoli/capillary membrane (increased distance gas has to travel between blood and alveoli) and a local fluid buildup (surfactant) within the alveoli. This produces a ventilation/perfusion mismatch that progressively worsens as more and more oxygen is delivered to a patient, becoming a precursor to the development of ARDS and pulmonary hypertension.
Oxidative Stress
Well, that all sounds horrible. But, there are even more insidious oxygen side effects that cause bodily damage. One of the culprits is a reactive oxygen species (ROS), which is a type of unstable molecule that contains oxygen and readily reacts with other molecules in a cell. Many of these are produced in the mitochondria as a by-product of the electron transport chain, making energy for a cell. All ROS are free radicals. Still, not all free radicals are ROS.5 Hypoxic cells are very susceptible, and ROS presence can exponentially increase damage – particularly of concern are the cells that makeup heart, brain, and lung tissue.
What’s a free radical, you say? It is an atom that has one or more unpaired electrons in its outermost shell.6 Oxygen has two pairs of electrons that are continually searching for a partner, thus making it a very potent and highly reactive free radical by nature. Free radicals bind with just about anything within the body with an electron and change their chemical structure, sometimes damaging them by stealing the electron.
The good thing is, the body has a built-in defense outside of the immune system that is specific to free radicals. These molecules are called antioxidants. Many are derived from fruit and vegetables (e.g., vitamins E and C and beta-carotene) and have “spare” electrons they can safely donate to free radicals, effectively satisfying them and turning off their urge to steal from other cells and tissues. Cell damage occurs when free radicals outnumber antioxidants, known as oxidative stress. The damage is directly proportional to the number of free radicals present at the site of injury.2. Thus, supplemental high-flow oxygen administration may very well induce further unnecessary tissue damage by flooding it with free radicals.
My Chest Hurts!
Now that you are aware of the potential consequences of prolonged high-flow oxygen administration let’s look at how this affects patients experiencing cardiac chest pain secondary to coronary artery disease. It’s been traditional practice to give high-flow oxygen, mainly via a non-rebreather mask, to these patients under the premise that it was helpful to a stressed, ischemic heart.
However, consider these three points of evidence: One study showed that hyperoxia reduced cardiac output by 10 to 15 percent in both healthy volunteers and patients with coronary artery disease, and, systemic vascular resistance was increased remarkably in patients with heart failure.13 Researchers in New Zealand found that, although evidence was limited, it suggested that routine use of high-flow oxygen in uncomplicated AMI may result in a greater infarct size and possibly increase the risk of mortality.6,10 Five minutes of supplemental oxygen by non-rebreather mask decreases coronary blood flow by 30 percent, increases coronary resistance by 40 percent due to coronary artery constriction, and blunts the effect of vasodilator medications like nitroglycerine.2,11
Why? Hyperoxygenation of the blood in the lungs displaces CO2 from hemoglobin, which then accelerates the rate of CO2 removal. If there is a significant decrease in serum CO2, this leads to vasoconstriction. If this happens in the lungs, pulmonary hypertension, and reduced oxygen delivery to the left heart develops. If it happens in the coronary circulation, decreased blood flow causes ischemia that progresses to injury, then eventually, infarct.
What if the patient presents with chest pain but has associated pulmonary edema? Eliminating all the contraindications, the obvious first choice for management is the application of CPAP. But remember, this setup can deliver up to 100 percent oxygen at a higher-than-normal positive pressure. The good news is, a study of prehospital non-invasive ventilation in patients with pulmonary edema and/or COPD, asthma, and pneumonia found that the use of CPAP with a low oxygen percentage of 28–32 percent was highly effective in the treatment of respiratory emergencies by medics.6,12 Thus, the patient may receive the benefit of CPAP, but not develop the hyperoxia consequences!
Backup
EMS professionals who are scared to withhold high-flow oxygen, believing that by doing so, worsens a cardiac patients’ condition. Regarding the studies mentioned, and the notion that more oxygen isn’t necessarily better, let’s look at the current American Heart Association Guidelines for Emergency Cardiac Care and CPR.
In 2010, AHA recommended: “There is insufficient evidence to support [oxygen’s] routine use in uncomplicated ACS. If the patient is dyspneic, hypoxemic, or has obvious signs of heart failure, providers should titrate therapy, based on monitoring of oxyhemoglobin saturation, to ≥ 94%.” 7 Jumping to the 2015 update, the updated care recommendations state: “The provision of supplementary oxygen to patients with suspected ACS who are normoxic has not been shown to reduce mortality or hasten the resolution of chest pain. Withholding supplementary oxygen in these patients has been shown to reduce infarct size minimally. In the prehospital, ED, and hospital settings, the withholding of supplementary oxygen therapy in normoxic patients with suspected or confirmed acute coronary syndrome may be considered “.8 Next year when the guidelines are updated, there may be even further evidence and change.
The 2017 DETO2X trial also lends support to decreasing the use of high flow supplemental oxygen, as it concluded: “The use of supplemental oxygen does not appear to offer any benefit to patients with acute myocardial infarction in patients with an O2 saturation > 90% “.9 Another conclusion from a 2019 study done in New Zealand concluded: “…in patients with suspected ACS who do not have hypoxemia, routine oxygen therapy provides no benefit and should therefore not be given.” 1
Conclusion
There are many reasons to avoid delivering prolonged, high-concentration oxygen. Nitrogen washout increased oxidative stress from free radicals, and alveolar damage from oxygen toxicity can all be prevented by flowing oxygen at a rate that maintains a SpO2 between 94 to 99 percent. If a patient is maintaining this level on their own, then no supplemental oxygen is needed. Given the current assessment tools, EMS professionals have the means to titrate oxygen therapy to patients’ needs, and those needs most often can be met by low-flow oxygen. A patient who needs oxygen should never be denied it – hypoxemia and hypoxia must be corrected! Just remember, you CAN have too much of a good thing.
References
- Hughes, S. (2019, September 3). Oxygen in Suspected ACS May Benefit Those with Low Levels. Retrieved from: https://www.medscape.com/viewerarticle/917611
- McEvoy, M. (2012, June 30). Can oxygen hurt our patients? Retrieved from: https://www.ems1.com/ems-products/cpr-resuscitation/articles/can-oxygen-hurt-our-patients-s2nMrrdQj297Inij/
- Callopy, K. (2011, December 11). Oxygen Toxicity. Retrieved from: https://www.emsworld.com/article/10523286/oxygen-toxicity
- Miller, B. E., & Hook, G. E. (1990). Hypertrophy and hyperplasia of alveolar type II cells in response to silica and other pulmonary toxicants. Environmental health perspectives, 85, 15–23. doi:10.1289/ehp.85-1568321
- Farnsworth, R. Oxygen: Not the Panacea You’ve Been Told. 2014. Powerpoint slide 13.
- Gandy, W.E., Grayson, S. (2013, April 4) More Oxygen Can’t Hurt…Can It? Retrieved from: https://www.emsworld.com/article/10915304/more-oxygen-cant-hurtcan-it
- Circulation, 2010; 122: S787–817.
- 2015; 132: S483–S500.
- Anand Swaminathan, “The DETO2X Trial: Do Patients with AMI Need Supplemental O2?”, REBEL EM blog, September 21, 2017. Available at: https://rebelem.com/deto2x-trial-patients-ami-need-supplemental-o2/.
- Wijesinghe M, Perrin K, Ranchord A, Simmonds M, Weatherall M, Beasley R. Routine use of oxygen in the treatment of myocardial infarction: systematic review. Heart, 2009; 95: 198–202.
- Harten JM, Anderson KJ, Kinsella J, et al. Normobaric hyperoxia reduces cardiac index in patients after coronary artery bypass surgery. J Cardiothorac Vasc Anesth 2005;19:173–5.
- Bledsoe BE, Anderson E, Hodnick R, Johnson L, Johnson S, Devendorf E. Low-fractional oxygen concentration continuous positive airway pressure is effective in the prehospital setting. Prehosp Emerg Care, 2012 Apr–Jun; 16(2): 217–21.
- Smit, B., Smulders, Y.M., van der Wouden, J.C. et al. Crit Care (2018) 22: 45. https://doi.org/10.1186/s13054-018-1968-2/